Abstract
Introduction: Natural killer (NK) cells are important components of graft-versus-leukemia alloreactivity after allogeneic hematopoietic cell transplantation (HCT) for leukemia, due to the inhibitory killer-cell immunoglobulin-like receptors (KIRs). Only NK cells expressing inhibitory KIRs to self human leukocyte antigen (HLA) can become licensed and more responsive to activating stimuli. However, NK cells with inhibitory KIRs for non-self HLA are proposed to exhibit transient alloreactivity after early allogeneic HCT. The inhibitory KIR2DL group of receptors interacts with HLA-C, which comprises two mutually exclusive groups: HLA-C1 (Asn80) and HLA-C2 (Lys80). KIR2DL1 receptor, which shows the most powerful inhibitory effect and is very frequently expressed in the Japanese population, recognizes the HLA-C2 group. Therefore, we studied combinations of donor and recipient HLA-C groups in children with acute leukemia who underwent unrelated cord blood transplantation (CBT) to clarify the impact of KIR2DL1 mediated-NK alloreactivity on clinical outcomes.
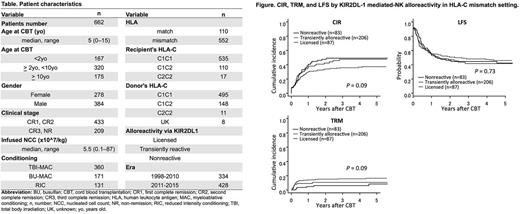
Methods: The current study was approved by the institutional review board of Japanese Red Cross Nagoya First Hospital in Nagoya, Japan. A total of 662 children aged 15 years or younger at the time of CBT with acute myeloid leukemia (AML, n = 261) or acute lymphoblastic leukemia (ALL, n = 401) who underwent first unrelated CBT between 1998 and 2015 in Japan were retrospectively analyzed based on the data from the Japanese Data Center for Hematopoietic Cell Transplantation. Patient characteristics are summarized in Table. We compared engraftment rate, cumulative incidence of relapse (CIR), transplantation-related mortality (TRM), leukemia-free survival (LFS), and grade II-IV acute graft-versus-host disease (g2-4 aGVHD) in association with KIR2DL-1 mediated-NK alloreactivity.
Results: Patients were divided into three groups according to the donor and recipient HLA-C status; licensedgroup (n = 92) with C1/C2 or C2/C2 donor and C1/C1 recipient, transientlyalloreactivegroup (n = 443) with C1/C1 donor and C1/C1 recipient, and nonreactive group (n = 127) with any donor and C1/C2 or C2/C2 recipients. Median follow-up of survivors was 45 months after CBT. There was no difference in engraftment rates at 50 days after CBT among the three groups, which was 91% for all groups (P= 0.83). The CIR/TRM/LFS at 3 years were 43%/7%/51% for the nonreactive group, 38%/12%/50% for the transiently alloreactive group, and 47%/10%/43% for the licensed group, respectively (P= 0.23, 0.29, and 0.50, respectively). The incidence rates of g2-4 aGVHD were 34%, 41%, and 47% for the nonreactive, transiently alloreactive, and licensed groups, respectively (P= 0.10). The CIR for transiently alloreactive group tended to be lower than those for the others, whereas the TRM for transiently alloreactive group was higher than those for the others; however, there was no difference in LFS among the three groups. Narrowing the cases to the HLA-C mismatch setting, the tendency of lower CIR and higher TRM for transiently alloreactive group became stronger. The CIR/TRM/LFS at 3 years in the HLA-C mismatch setting were 49%/6%/45% for the nonreactive group (n = 83), 36%/16%/48% for the transiently alloreactive group (n = 206), and 48%/11%/41% for the licensed group (n = 87), respectively (P= 0.09, 0.09, and 0.73, respectively, shown in Figure). The trend of lower CIR and higher TRM for the transiently alloreactive group remained unchanged for both AML and ALL patients.
Conclusions: There was a significant association between transient KIR2DL1-mediated NK alloreactivity and reduced CIR after HLA mismatch CBT for childhood acute leukemia, which suggests improved LFS with efforts to reduce TRM. Further large studies are warranted.
Atsuta: Otsuka Pharmaceutical Co., Ltd.: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal